Clinical trial optimization is the key to setting your research up for success.
- Are you wondering how to improve patient recruitment and retention?
- Unsure about how to streamline trial phases without compromising data quality?
- Feeling overwhelmed by the sheer magnitude of data management?
Good news: this article has some answers.
With over a decade of assisting a wide variety of research projects, we know how to optimize study communication through the development of customized solutions for research teams.
This article is perfect for:
- Clinical trial managers aiming for more efficient processes.
- Research professionals striving to maintain data integrity.
- Medical practitioners invested in enhancing patient experiences during trials.
The issues that clinical trials face in terms of efficiency arise long before many chemicals even make it to human testing. The decentralized and complex, multi-disciplinary nature of clinical trials leads to countless opportunities for redundancies and inefficient practices.
The quality of data used and the lack of appropriate communication channels compound the issue of efficiency and contribute to the shockingly high failure rate of therapies trialed in human participants.
Here, we discuss some of the major issues faced by modern clinical trials and go into some of the ways in which clinical trial optimization at various stages of the process can contribute to higher-quality therapies and less expensive and wasteful clinical trial planning and execution.
What’s The Drive Behind Clinical Trial Optimization?
Clinical trials are multiple-staged, multifaceted endeavors that cover many years, sometimes even decades, when taking preclinical trial stages into account as a precursor. With so many steps and industries involved, there are multiple opportunities for optimization and a high amount of pressure from many angles to make the process more efficient overall.
Clinical trials themselves take many forms. While the process is similarly split into phases for each type of research, there are different challenges at different stages for cancer trials, for example, than with trials for diabetes drugs.
Each phase of a trial costs more than its predecessor, with phase one trials costing on average around $4 million, phase two trials commonly reaching $13 million and phase three costing an average of around $20 million. Depending on the study, phase 4 of the trial can cost up to $39 million.
Each phase commonly takes multiple years to complete, and almost all trials end in failure at some stage of this process. This means that in to bring a single drug to market, there is a median capitalized R&D cost of $985 million.
These costs reflect the money lost in all the failed tests and therefore represent a strong motivation to improve the process and cut down on failure rates. Better procedures, more streamlined processes, and more accurate modeling, communication, and data collection will all contribute to faster, more effective, and ultimately more affordable treatments for all types of treatable health conditions.
5 Common Clinical Trial Challenges
In order to refer to potential solutions to roadblocks in clinical trial execution, it’s a good idea to identify some of the challenges first. These challenges come at almost every stage of the trial, but we’ve listed five points of discussion, at which optimization could dramatically increase the efficiency of the clinical trial process:
1 – Ethical and Logistical Issues with Animal Testing
Animal testing is a lengthy process that often fails to predict a drug’s suitability for human use. Ethical concerns and physiological differences between animals and humans lead to high failure rates after costly study phases.
2 – Mismatched Incentives Between Sponsors and Trials
Finding sponsors is a significant challenge. Misaligned incentives between sponsors and clinical teams create delays in funding agreements, damage relationships, and slow down trial start-up.
3 – Finding Suitable Patients
Many trials struggle with low sample sizes, particularly in areas like cancer research. Finding patients who are a good fit for a trial is both time-consuming and expensive, often leading to delays.
4 – Difficulties in Patient Retention
Patient retention is a critical issue. Factors like hospital time, access to trial results, and relationships with investigators influence whether patients stay involved, and poor retention can collapse entire trials.
5 – Follow-Up and Post-Treatment Data Collection
Follow-up data collection is often poorly planned, with many patients dropping out. Without adequate resources and strategies in place, gathering accurate data post-treatment can be highly challenging.
Pre-Clinical Trial Optimization
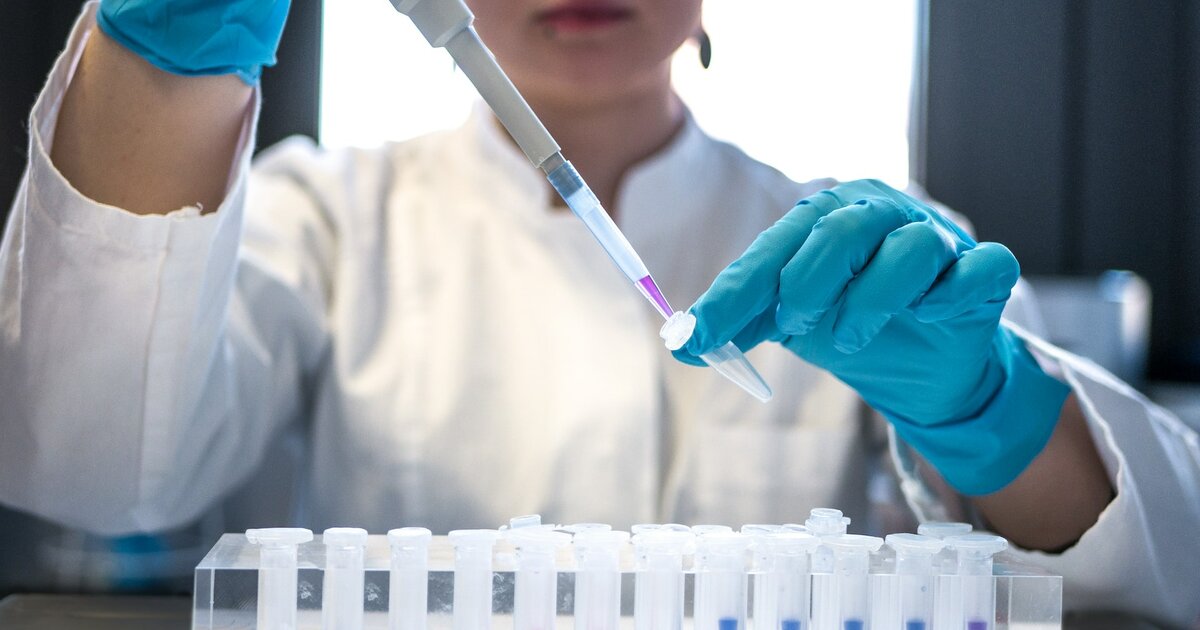
Before human testing can begin, a compound must undergo up to six years of pre-clinical trials. Only 2.5% of compounds make it to the animal testing phase, and only 7% of those proceed to human trials. This lengthy process consumes significant resources, and optimizing clinical trials at this early stage is crucial. Reducing the time and resources needed to identify promising compounds could greatly enhance the overall efficiency of clinical trial optimization, ensuring that only the most viable candidates move forward.
AI is playing an increasingly important role in this pre-clinical phase, particularly in predicting a drug’s effectiveness and toxicity before it reaches human trials. Utilizing AI-driven models allows researchers to streamline compound selection and recruitment processes, helping to optimize clinical trials. This technology not only predicts the success of drug candidates but also identifies suitable patient populations earlier, ultimately reducing failure rates.
Moving Beyond Animal Testing
Animal testing has long been a cornerstone of drug discovery, but it is both ethically controversial and scientifically limited due to the physiological differences between animals and humans. Finding alternatives to these outdated methods is a key component of optimizing clinical trials. Emerging technologies, such as microfluidic culture devices and AI-driven simulations, are offering viable replacements. These new approaches not only reduce ethical concerns but also provide faster, more accurate results that align better with human biology.
Clinical trial optimization is advancing with these innovations, paving the way for more efficient testing. AI models, for example, can simulate human responses, predicting potential outcomes without the need for animal subjects. This results in more ethical, time-efficient, and cost-effective trials.
Optimizing Clinical Trial Planning
The planning phase of clinical trials involves numerous stages, each with deadlines and tight budgets. Delays at one stage often cause a ripple effect, leading to inefficiencies throughout the entire trial. Effective clinical trial planning must address these issues to prevent delays. Automation and integrated data systems offer solutions to streamline negotiations and eliminate bottlenecks, enabling trials to progress more smoothly.
More efficient planning leads to a faster, more cost-effective trial process overall, benefiting both researchers and patients. Clinical trial optimization at this stage is crucial for maintaining momentum in later phases.
Running Clinical Trials More Effectively
Logistical challenges frequently arise once a trial begins. Resource misallocation and patient retention issues are just a few of the factors that can hinder progress. Implementing strategies to overcome these obstacles is vital for optimizing clinical trials during the execution phase. Mobile research units that bring trials directly to patients’ homes are one innovative solution. This not only improves patient retention but also reduces overall costs by minimizing the need for hospital visits.
Advances in communication software and wearable devices are enhancing remote monitoring, ensuring that data collection remains accurate and consistent. Addressing these logistical issues ensures trials run more efficiently and with greater success.
Enhancing Follow-Up Stages
Follow-up data collection is a crucial component of any clinical trial, yet it is often neglected during the planning stages. Poor follow-up strategies can lead to costly dropouts and incomplete data sets. Improvements in follow-up procedures must be a priority in optimizing clinical trials. Remote devices, combined with communication apps like Mosio, keep patients engaged. Automated reminders and text surveys ensure that participants remain active, even in the later phases of the trial.
These tools allow researchers to gather the necessary data without excessive time and resources spent chasing patients, making follow-up stages more efficient and cost-effective.
Getting Started with Mosio
Mosio serves as a key solution in clinical trial optimization, especially in improving patient engagement and retention. Its automated communication tools help keep participants involved throughout the entire trial process, from recruitment to follow-up. Features such as timely reminders, personalized medication schedules, and customized text surveys simplify data collection, leading to reduced dropout rates and more accurate results.
With Mosio, research teams can improve communication with participants, resulting in a more efficient and streamlined trial experience. The platform enhances patient retention while minimizing the resources needed for follow-up, making that phase significantly more effective. As the field of clinical trial optimization advances, tools like Mosio will become essential for increasing trial efficiency and speeding up the development of cost-effective therapies.